Get new exclusive access to healthcare business reports & breaking news
Thousands of tasks happen behind the scenes every day in hospitals and clinical organizations. Countless staff members handle email, call logging, scheduling, patient intake, and billing. Over time, departments become hyper-focused on their own responsibilities and lose sight of how work actually moves between teams.
The result: a nurse spends 20 minutes tracking down a discharge summary that three departments thought someone else owned. Prior authorizations sit in shared inboxes because no one knows who’s responsible. A follow-up call never happens because two people assumed the other made it.
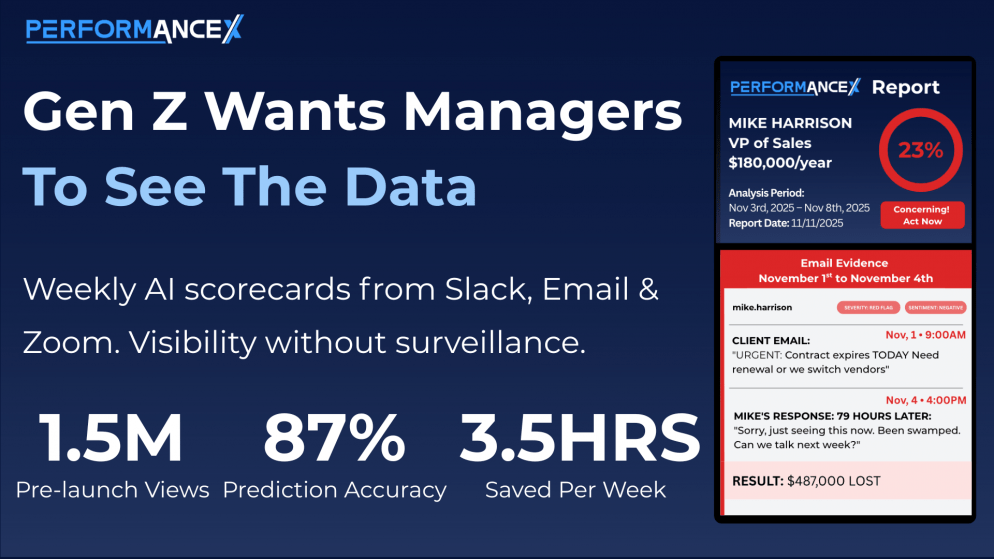
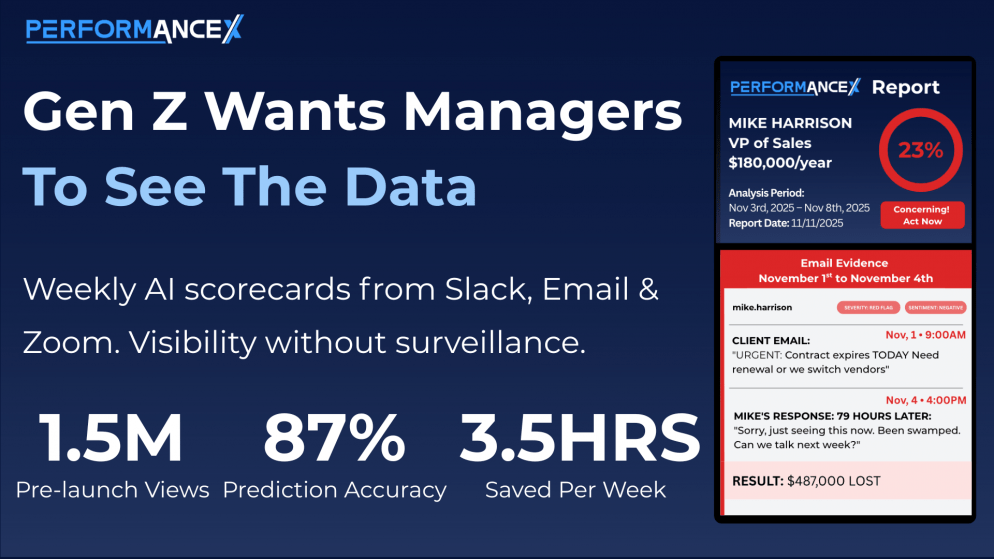
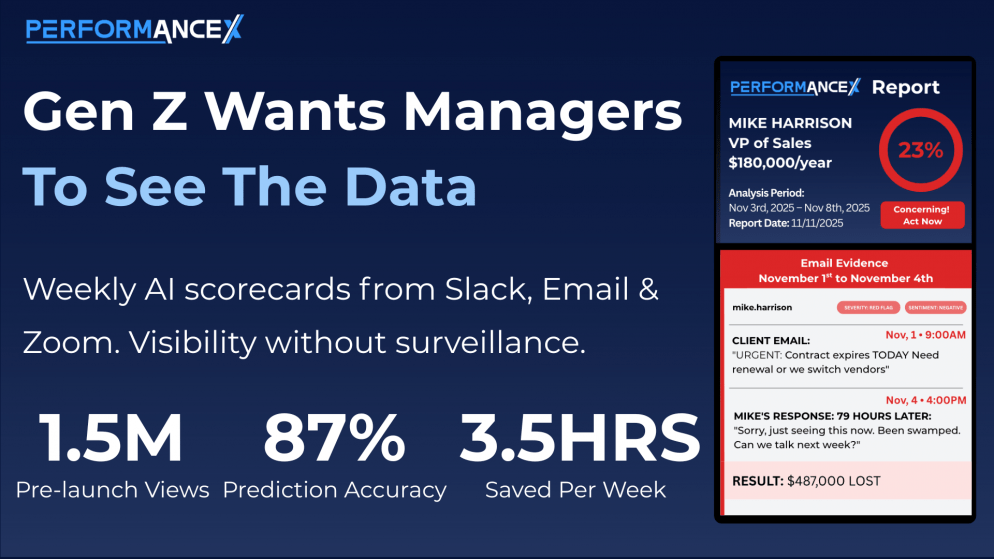
While more tools might seem like a good option, what hospitals actually need is proof of what’s happening — who’s doing what, where work stalls, and which handoffs are failing. That’s what PerformanceX delivers: not more dashboards, but evidence of how work actually gets done compared to how the organization thinks it gets done.
For years, hospitals have leveraged technology as a trusted partner to enhance workflows and improve patient care. But most analytics tools summarize metrics after the fact. They tell you what happened last quarter. They don’t show you the prior authorization that’s been sitting untouched for 72 hours right now.
AI performance monitoring is different. It connects to the tools staff already use — emails, chats, phone recordings, scheduling platforms, intake tools — and shows leaders exactly where work is stuck, who’s overloaded, and which tasks are falling through the cracks.
There’s no migration. No new software for staff to learn. The system reads the work employees are already doing and converts it into weekly reports, complete with names, timestamps, and supporting evidence.
Leaders see workload distribution across individuals and teams. They know what’s causing delays. They identify tasks that require attention before they become expensive problems.
Hospitals continually look for better ways to manage their core operational functions:
These may seem like small tasks, but they significantly impact patient wait times, procedure authorizations, and continuity of care.
A 2025 report found that many clinicians spend nearly 90 minutes a day on administrative work — time that could otherwise go to patient care. Research also highlights burnout among clinicians, which leads to staff turnover, less efficient care delivery, and increased costs for health systems.
The problem isn’t effort. It’s that leaders can’t see where effort is being wasted.
AI-powered assistants and workflow tools can automate tasks and increase administrative efficiency. But automation only helps when you know what to automate. Performance monitoring shows you where work breaks down so you can fix the right problems:
With this evidence, leaders can redistribute workload, adjust staffing, and support more balanced operations — based on facts, not assumptions.
Leaders see missed calls, slow response times, delayed follow-ups, and scheduling gaps — with timestamps showing exactly when each happened. Teams can pinpoint where patients are waiting too long and fix the specific breakdown causing it.
The data shows documentation delays and communication overload that would otherwise go unnoticed. When leaders can see who’s drowning before they quit, hospitals can reduce burnout and improve patient transitions.
Weekly reports show recurring denial types, follow-up gaps, and payment delays. Teams can address root causes instead of chasing the same problems month after month.
Managers get objective data on workload distribution — who’s carrying too much, who’s underdelivering, and where staff need support. This allows for balanced staffing decisions and coaching based on evidence, not perception.
Leaders see a unified view of operations affecting staff and patient care. No more waiting for quarterly reports or exit interviews to learn what’s broken. Weekly evidence supports faster decisions and more predictable outcomes.
Hospitals generate more operational data than ever before. The problem is that it’s scattered across dozens of tools and nobody’s connecting it.
Performance monitoring closes that gap by turning everyday work into a unified, evidence-based view of what’s actually happening. Leaders see their operations clearly. Teams collaborate better. Managers make faster decisions. And leadership can focus on improving patient care — instead of chasing data that should have been obvious weeks ago.