



Get new exclusive access to healthcare business reports & breaking news




Telemedicine is a fairly new digital health discipline that continues to make the lives of providers easier, drive healthcare access, and deliver better patient outcomes. It’s also one area of medicine that is growing at an epic pace, causing a seismic shift across the healthcare spectrum.
Latest data shows that telemedicine market size is anticipated to grow at a compound annual growth rate (CAGR) of 19.2 percent to hit over $130 billion by 2025, up from $26.5 billion in 2018.
There’s a lot happening on the telemedicine front, and it pays to keep up with these exciting changes, breakthroughs and the impact it’s having on healthcare.
This is the most authoritative guide you’ll ever read, covering everything you need to know about telemedicine.
Telemedicine is a collective term for the usage of digital avenues and a series of other telecommunication technologies to facilitate long-distance healthcare access for patients and improve the quality of care.
It involves the use of technologies like the internet, wireless & terrestrial communications, video conferencing, chatbots, streaming media, and other digital channels. The goal is to support the connection between doctors and their patients without the need for face-to-face meetings.
As such, telemedicine is transforming, public health, medical research, professional health-related education, and healthcare administration.
More specifically, this emerging concept in digital health enables doctors and other healthcare professionals to leverage robust telecommunication tech to remotely diagnose disease, offer treatments and prescribe medication.
Originally designed to serve patients in remote areas (think people seeking health care in remote flanks of Alaska), telemedicine has over the years burgeoned to cover patients who don’t necessarily live out of reach of a conventional hospital.
The allure behind telemedicine is its ability to provide convenience for the doctors and patients alike. The value comes from the fact that patients no longer have to wait through long queues in a doctor’s office. From chatbots to 24/7 AI availability – this contiguous service allows patients to get in touch with healthcare providers without having to make any trip to the hospital.
With that being said, telemedicine has experienced unprecedented evolution in the past decade or so, and it’s becoming a core part of the US healthcare infrastructure. With experts predicting that the market will reach more than $130 billion by the year 2025, we are yet to see the best of telemedicine.


Despite gaining traction in the past few years, modern telemedicine applications have been around primarily since the 1950s. It all started when a handful of American university medical centers and top-tier hospitals have begun looking for ways to reach patients in remote locations, as well as share medical information (most notably images) via telephone.
Interestingly, however, some rudimentary forms of telemedicine use can be traced back to the turn of the 20th century in Europe. Willem Einthoven, a Dutch physician, is often credited for being the first health professional to transmit electrocardiograms over a long distance in 1905. It was not long before other physicians in other European countries followed suit.
Even before then, Lancet featured an interesting article that talked about leveraging the convenience of the telephone to reduce unnecessary doctor’s visits.
Between 1920 and 1940s, there were several radio consultations carried out from medical centers in France, Italy, and Norway for patients in remote islands/hard-to-reach area and those onboard ships in the high seas.
To get a holistic view of the fascinating history of telemedicine, we might want to take a step back. Over the years, telemedicine has made huge strides and milestones thanks to the proliferation of telecommunication technologies. At the very start, telephones and telegraph made it possible for the public to make long distance communication.
While the telegraph was a reserve for a section of the community because of its complications, the telephone took center stage in the maturity of telemedicine. Nonetheless, thanks to the speed of delivery of telegraph, the telecom tech was often used in a military environment.
For instance, during the American Civil War, soldiers and commanders took advantage of the telegraph to make orders for medical suppliers. Some of them send telegrams to communicate injuries and casualties on the battlefield. There’s also some evidence that the military doctors might have used the telegraph for medical consultations.
It’s the telephone, however, that brought the world of the connection to the mainstream. The telefax, which incidentally was developed before the telephone, didn’t participate in telemedicine until the fax machines were wired to telephone lines. To this very date, some health providers still use faxes to transfer medical information.
Several attempts to kick-start telemedicine were made in the early and mid 20th century. In 1925, for example, Dr. Hugo Gernsback imagined a device called teledactyl whose illustration was featured on the cover of the Science and Invention.
In the mind of Dr. Hugo, the futuristic device would use radio technology, TV and robotic fingers to assess the patients and relay the information to the doctor. While Dr. Hugo’s idea didn’t come to fruition, it depicted telemedicine is what it would become today – a remote video consultation with the physician.
Fast forward to 1948, when two eastern Pennsylvania-based medical centers 24 miles apart exchanged radiologic images using a telephone. This spur a trend in the 1950s whereby research and medical centers started experimenting and putting the idea of telemedicine into practical use.
From this point on, telemedicine took a rollercoaster ride dotted with breakthroughs, challenges, and risks. Here’s the timeline:
1959: Examiners at the University of Nebraska started using interactive telemedicine to share neurological tests with their students. At about the same time, radiologists in Canada offer telemedicine-based diagnostic consultations via coaxial cable.
1960: Psychiatric consultations are carried out over a CCTV link between Norfolk State Hospital and Nebraska Psychiatric Institute.
1961: Journal Anesthesiology publishes a report on the possible use of radiotelemetry to monitor patients.
The 1980s: Telemedicine consultations makes it easy for radiologists to receive images via teleradiology systems.
The 1990s: The onset of the internet age provides an avenue for web traffic and ushers in the ability to share information at an incredible speed, and to a wider audience.
Today: The period since 2009 has been an interesting and equally rewarding time for telemedicine stakeholders. Initiatives like the HITECH Act and ARRA have helped catapult MedTech and drive digital health to the next level. Of course, there have been several acts and regulation frameworks enacted to protect patient interests and pave the way for more robust telemedicine.
Take the Patient Protection and Affordable Care Act of 2010, for example. It set the pace for creation of ACOs, an approach to healthcare whereby remote patient monitoring and telemedicine are the order of the day.
Other well-meaning initiatives like the HRSA’s award of $16 million to improve access to healthcare in remote/rural communities has helped spur the growth of telemedicine.
On the overall, snappy internet connections, the proliferation of mobile ecosystem, and the push to improve the quality of care are a perfect combo for an environment that telemedicine will thrive. And it has for the most part, but not without challenges, risks, and opportunities (more on this ahead).
By definition, telemedicine is an approach of medicine whereby technology and information are used to deliver or support long-distance care. In layman terms, this refers to a medical practice in which the healthcare professional in one location uses the internet, mobile or other telecommunication technologies to examine, diagnose and treat a patient located offsite.
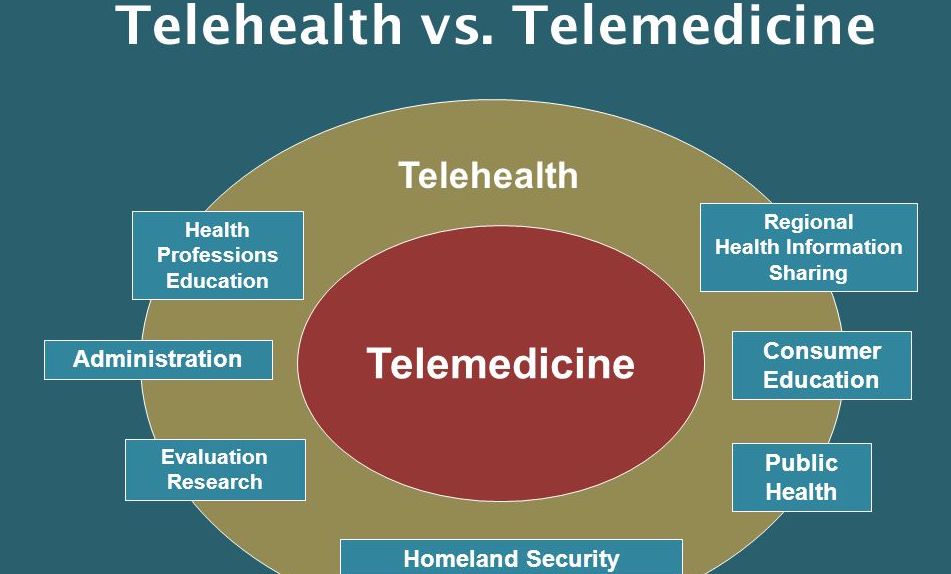
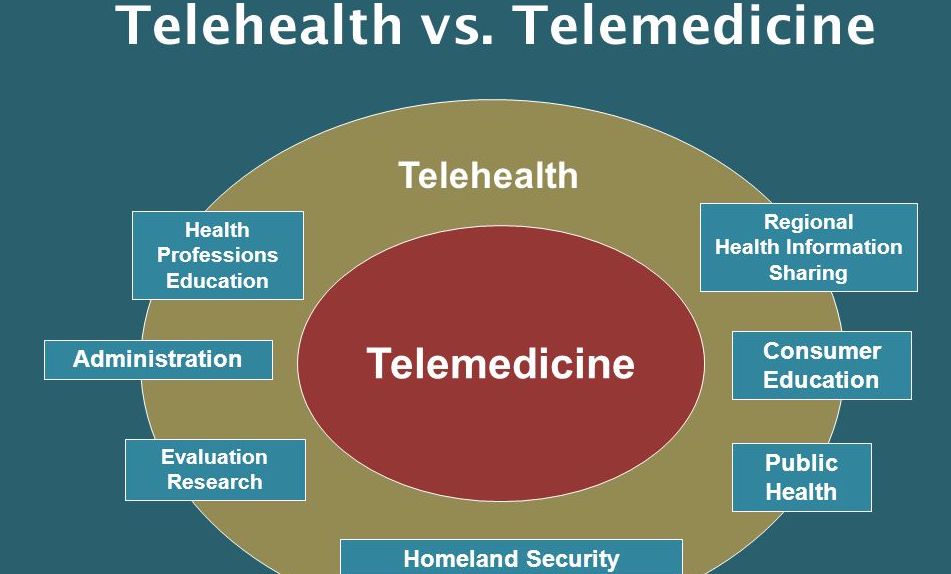
Telehealth, on the other hand, encompasses all methods, means, and avenues for enhancing public health, medical education and healthcare support and delivery using telecommunication technologies. In other words, this refers to a collection of services, telecommunication technologies, and electronics used to provide or support long-distance healthcare.
If you dig deeper, you will notice that telemedicine is actually a subset of telehealth, which is a broader term which covers a wider scope of long-distance healthcare service. In practice, telemedicine often has to do specifically with the clinical or diagnostic services offered by doctors for at-a-distance patients. Most telehealth services are non-clinical in nature.
Although both fields of healthcare make use of the latest technologies like Electronic Health Records (EHRs), remote patient monitoring, wireless health technologies, video conferencing, etc., the key difference lies in the scope.
In most cases, telemedicine solutions are designed for remote specialist/physician consultation, medication adherence, managing chronic conditions, and follow-up visits. Telehealth technology, on its end, is frequently used for non-diagnostic/non-clinical services like offering continuing medical education, managing doctors schedules, administrative meetings, and medical training.
Of course, there are many areas of overlap and intersection between the two emerging concepts in modern medicine. Here are a few examples to drive the point closer home:
A video conferencing app that supports continuing education for nurses is a telehealth solution, whereas a similar platform that allows physicians to check up on their patients after a visit is considered part of telemedicine.
Similarly, a medical software that enables a primary care physician to send images of skin blemishes to a dermatologist at a different location can be classified as telemedicine. On the flipside, an app that alerts the public to a disease outbreak is a telehealth app.
In saying that, it is not wrong to say that telemedicine is directed almost always at the patient. Telehealth is perhaps designed to support and enhance the entire healthcare system, from provider training and solution development to patient care and support.


It is estimated that an average doctor’s office visit cost around $146. But telemedicine services cost approximately $79 per visit on average, according to a recent report.
The bigger question now becomes: is telemedicine covered by medical insurance plans? How much can you expect to be reimbursed?
The coverage for telemedicine is largely influenced by regulations and laws at both the state and federal, as well as the policies of specific insurance companies. In fact, the amount of telemedicine reimbursement typically varies from state to state, depending on their legislation.
A number of states have made it mandatory for private insurers to reimburse the same amount for telemedicine services as they’d for in-person hospital visits. But there’s still some grey area for payers. Although most states do so, they often leave it to the health insurance companies to determine the amount of reimbursement.
As of today, there are 26 (and counting) states that have regulations and laws in place that mandate private payers to reimburse providers for telemedicine services. These state laws are usually referred to as “parity laws.” The name owes to the fact that regulations are not the same for two given states.
There are 10 more states with telemedicine laws baking in the oven. The overarching principle behind each telemedicine regulation is that health insurance may not discriminate based on the patient’s location.
There are a few exceptions, though. Small group HMOs and worker’s compensation insurers might have leeway to not offer telemedicine coverage. The good news is that the vast majority of private insurance companies, Medicaid and Medicare reimburse telemedicine services at the same level to doctor’s office visits.
Telemedicine solutions provide patients with an effective and convenient way to receive remote consultations, diagnosis, treatments, and much more from vetted healthcare professionals. The icing on the cake is that they don’t have to leave the comfort of their workplaces or homes. But, how does telemedicine systems work anyway?
There are many situations in which telemedicine is an excellent option to get care or seek medical advice. First off, there are those occasions when the patient knows what they have, and there is no need for an in-person visit with a doctor.
Often, the patient might have specific medical questions, whether about their condition, medication or general knowledge. As you already know, a simple web search may return lots of misinformation that can lead to grave ramifications for the patient’s health and wellbeing.
Previously, healthcare providers used telephones, fax devices, and telecoms to facilitate telemedicine. The spread of the internet, however, has greatly changed how telemedicine works. Patients in remote and rural areas can now use their internet connection to take part in several types of telemedicine.
Here’s a sample model of how telemedicine works
Step 1. Pick the right telemedicine solution for you. Most of these solutions are web-based services or mobile applications. They help make it easy for physicians to connect with patients remotely. Not just that – they can also gather, store and process patients’ medical information for ongoing care. As such, the next step would be to install a mobile app or sign up for an online account with a telemedicine platform.
Step 2. Set up your profile. When creating an account with a telemedicine solution, you need to provide personal information like your age, name, date of birth, phone number, email, etc. Of more importance, you have to provide a brief health history, allergies and other nuggets of information that the physician could use for diagnosis and deliver the right treatment.
Step 3. You are ready to get telemedicine services! At this juncture, you can request a consultation with a physician, ask health-related questions, and discuss your personal health issues with a trusted medical professional.
Depending on the telemedicine solution, you can text, chat, or video conference a physician. The healthcare professional can request for supporting images. For instance, you can take photos of your rash and upload them for the doctor to review.
With telemedicine, care doesn’t stop right after the consultation. You can hold several follow-up sessions, request prescriptions for medication, and much more in between.
There are several forms of connections that facilitate and support telemedicine platforms, solutions, systems and services. These include:
E-health Patient Services Websites: This is the most common type of telemedicine connection. Web-based software platforms or account-centric sites connect patients to doctors for care and outreach service online.
Monitoring Center Connections/Links: This is a type of telemedicine connection that powers remote monitoring of patients. In essence, the links establish connections between a remote monitoring center and the home/residence of a patient. These links make it easy to monitor the vitals of a patient remotely and share the date with relevant healthcare facilities and providers.
Often used to monitor the patient’s fetal, cardiac and pulmonary data, monitoring center links can come in the form of text, web or telephony connections.
Point-to-Point Connections: Sometimes called point-2-point connections, these types of telemedicine connections create a link between a big (mostly urban) healthcare facility/hospital to small health centers/clinics in rural or remote areas. This allows understaffed or ill-equipped small hospitals in rural sites to include specialists in bigger, more advanced healthcare facilities to offer better care to remote patients.
Often established via high-speed internet, these connections often apply to urgent care, teleradiology and telepsychiatry services especially for veterans in rural sites.
Networked Programs: This type of telemedicine program commonly established a high-speed internet connection link between a tertiary health facility like state general hospitals and community health and outlying clinics in remote areas. According to a recent report by the American Telemedicine Association, there are over 200 such programs in America, helping perk up over 3,000 outlying health clinics in remote areas.


The CCHP (Center for Connected Health Policy) is one of the key bodies that are at the forefront of making telemedicine go to the mainstream. The center put categories telemedicine into 4 major types – namely mobile health platforms, real-time interactive services, store & forward services, and remote patient monitoring.
Each type of telemedicine play a unique role and can offer a myriad of benefits to healthcare organizations, providers and patients alike. Let’s take a closer look at each, shall we?
This is the fastest growing type of telemedicine, and justifiably so. The mobile is one of the most intimate and convenient technology platforms thus far. In fact, there’s a growing trend of patients getting involved in their own health care. Most of them use their tablets, smartphones, wearables and other mobile devices to monitor and try to stay on top of their health and wellness.
It was only a matter of time before healthcare stakeholders developed telemedicine solutions for the mobile ecosystem. These solutions are collectively part of mobile health (mHealth platforms.
Mobile health solutions hinge their efficacy on mobile applications and software to support telemedicine and healthcare as a whole. There are many mHealth apps already in use right now, ranging from senior care apps to diabetes management mobile systems.
This type entails instant interaction between the patient and a healthcare provider. Video chat, video conferencing and live chat features enable real-time interactions that allow healthcare professionals to diagnose and treat disease, as well as offer medical advice to patients remotely. They can use other media avenues like social media and proprietary online communication platforms.
This type of telemedicine is often geared towards non-urgent care services, treating common ailments that don’t require the patient to go to a doctor’s office and delivering psychiatric evaluations. The beauty of these real-time interactive services is that they offer the appeal of a one-on-one doctor’s appointment without the added costs and travel.
Here are some of the top examples of live interactive telemedicine services:
This sometimes known as asynchronous telemedicine. It refers to a telemedicine system in which recorded medical history is transmitted to a doctor, physician or other healthcare providers. The idea here is that the provider uses the recorded patient information to diagnose or offer treatment outside of real time.
This type of telemedicine usually applies to specialist healthcare professionals who are in high demand and therefore not always available real-time interaction. That’s why it has become a popular type for understaffed facilities in rural and remote areas.
Also referred to as self-monitoring or self-testing, remote patient monitoring is a type of telemedicine that leverages a variety of telecommunication technologies to monitor vitals and other health signals of a patient remotely.
To that end, solutions that fall under this category are often used to monitor and effectively manage chronic and intensive-case conditions like heart disease, diabetes, asthma, and so forth. The draw of remote monitoring is clear: it’s cost-effective, convenient, and can allow for frequent (if not 24/7) monitoring.


Counseling and therapy are typically non-urgent areas of psychological medicine, which usually require ongoing interaction, follow-ups, and monitoring. This makes telemedicine an ideal solution.
With a consistent shortage of qualified psychiatric professionals, online counseling and therapy sessions can come in handy. Patients don’t have to waste time waiting at the provider’s office. More importantly, the mental health provider can make use of small chunks of free time to offer services to at-a-distance patients.
Tele-therapy and tele-counseling services provide the patient with the intimacy of an in-person session, all without having to leave the comfort of their own home. Consequently, patients can always schedule psychiatric appointments on short notice for situations that aren’t too urgent. The benefits include cost savings, better use of the provider’s time, and a reduced number of walk-ins and no-shows.
Diagnosing dermatology issues like acne, rashes, eczema, skin blemishes, and whatnot is highly visual. And usually, most of these conditions require photographic evidence or observational diagnosis. Rarely do dermatologists need a lab test or radiological examination?
That’s why teledermatology is a fast-growing area of telemedicine. In fact, industry experts think the future of dermatological exams lies in remote diagnosis.
There is already a growing list of mobile-based dermatological solutions such as dermoscopy. These telemedicine apps can help dermatologists examine patients and diagnose skin issues faster. This is especially true for patients who reside in rural and remote sites. The visual nature of telemedicine sessions makes it easy for modern providers to do their job.
Cold and cough-related ailments are common across the US. While they can be a nuisance, a cough can be diagnosed and treated without the patient having to visit the doctor’s office. That’s why more and more people are encouraged to use telemedicine platforms when they suspect they have a mild cough or cold symptoms. These include a runny nose, slight fever and coughing.
Because coughs can spread germs, it is prudent for the patient to get a consultation and receive a prescription right from their homes. This way, they can get the rest they need, and make sure they don’t pass it to others.
The good thing about diagnosing cough or cold is that the symptoms are very clear. However, the provider will take advantage of the interactive nature of telemedicine to carry out a preliminary screening by asking common questions. It is through this approach that the doctor will establish if the cold or cough is something serious like pneumonia or influenza.
If it is indeed serious, the doctor will urge the patient to go for further examination. If it’s something mild, the patient will get an e-prescription so that they can pick up their cold medicine from a local pharmacy or drugstore.
Access to specialist cancer care is usually limited or unavailable in remote or rural areas. That’s where telemedicine can come in handy. In specific, teleoncology can help improve both the quality and access to top-notch cancer training, education, support and care.
If applied properly, teleoncology has the potential to offer cutting-edge solutions that will help specialists deliver cancer solutions to patients in areas where the healthcare facilities are understaffed or lack oncologists.
These telemedicine solutions have the capacity to increase the survival rates of patients with cancer and help live fruitful lives regardless of their locations. Oncologic services can be offered through one-way or two-way interactions between the oncologists and the patient via store-and-forward or live technologies.
Low blood pressure associated with certain types of diabetes requires constant monitoring of the patients. With the proliferation of remote patient monitoring solutions, however, it was just a matter of time before patients with low or high blood pressure (hypertension) use telemedicine to manage their conditions.
It certainly makes sense to use monitoring devices and schedule regular online visits with the cardiologists or physicians. This is by far more convenient and cost-effective than making frequent trips to the doctor’s office.
If the physician determines that the patient needs urgent attention and care, they can get in touch with emergency medical technicians for immediate intervention. Telemedicine works well in tandem with today’s wearable devices and portable blood pressure takers that can transmit patient data directly to the doctor.


The work of a surgeon doesn’t end after the patient is discharged. They have to follow up with the patient to ensure that they are resurging well and to assess their progress. Having the patient make a trip to the surgeon’s office after a surgical procedure can be costly, time-consuming, and a great inconvenience.
That’s why telemedicine is a no-brainer for post-surgery follow-ups. It can save everyone money, time and lots of hassle in the long haul. By using video follow-ups, the patient can take plenty of rest they need to recover, the progress can be monitored frequently, and offer more social support and family involvement.
For the surgeon and their teams, this can present a great way to boost productivity, peer review, and collaborative opportunities. Good thing, research has shown that telemedicine and other digital health solutions can cut readmission rates for hospitals, one of the Medicaid ranking factors.
Filling and refilling medication prescriptions are big time-wasters for both the patient and the physician. Telemedicine may be what the doctor prescribed (pun intended!)
That’s right; healthcare providers can take advantage of the convenience of telemedicine to issue prescription refills. All the patient has to do is use an app or print out a prescription and take it to a local drugstore or pharmacy.
It is worth noting that telepharmacy and e-prescriptions may be restricted in some states and local jurisdictions. As such, it is up to the doctor to check if it telemedicine is allowed for prescriptions in the state where the patient resides.
Most digestive problems are non-urgent and can be handled by the doctor through telemedicine. Gastrointestinal issues like acid reflux, constipation, lactose intolerance and bloating don’t need a great deal of intervention from a healthcare professional.
Patients with mild gastrointestinal issues can consult with a doctor via telemedicine to zero in on the cause of distress. Whether it is a symptom for another health problem, medication side effects, stress-related or dietary caused, the doctor can recommend the best OTC medication to take care of the issue.
Telemedicine can help people with digestive problem spend less time from work, family or whatever matters to them. They don’t have to beat the traffic to reach a doctor’s office only to be told that it medication they are taking that’s causing their problem. They can also benefit from less stress involved with finding the right clinician for the problem.
Addictions, no matter the kind, can be devastating on the patient’s physical, emotional and mental well-being. Some addiction issues need urgent care, while others need routine follow-ups. It is patients that belong to the latter camp that can benefit from telemedicine.
Patients can receive counseling and psychological assessments via telemedicine. When they feel that they are almost falling back to their old habits, they can use telemedicine platforms to seek immediate help and support.
Most telemedicine systems also offer a network of support for patients with addictions. This platform gives them the right tools and people they can share coping skills and tactics.
Pediatric doctors deal with a ton of cases of sore throats almost every day. When flu, cold or virus hits a daycare, the pediatric physician will have their practice filled with little ones experiencing sore throats.
This is especially a condition that telemedicine can do the trick. Why? Because sore throats are caused by infectious and contagious viruses, it is important to keep those infected from the public. This will help keep the virus from spreading to other vulnerable kids.
The other big advantage is that telemedicine allows busy parents to have their kids’ sore throats checked by vetted healthcare professionals at the most convenient time, which is usually in the morning or evening. The doctor will use video chat or other telemedicine channels to determine if a sore throat is serious or not. If it needs further investigation, the doctor will call in the patient. It is that simple and hassle-free!


Right off the bat, it is worth noting that Medicare has for long recognized the importance of telemedicine in terms of healthcare access. However, reimbursement for telemedicine services can be quite tricky through Medicare. But it is not all gloom and doom.
In the early days of telemedicine adoption, Medicare recognized and reimbursed only a few and specific telemedicine services. Needless to say, there were lots of strict requirements. However, over the past handful of years, the telemedicine space has made huge milestones, and so as Medicare’s opinion of the industry.
Medicare now has a long list of reimbursable health services offered through telemedicine. That, however, has done little to the restriction the public payer imposes. Let’s dig a little deeper into what you need to know about Medicare and telemedicine.
As per Medicare guidelines, the location of the patient at the time of medical service is the Originating site. The health provider’s location at the time of delivering service is what’s defined as the Distant site.
While Distant site is subject to a few restrictions, it’s the Originating site that Medicare is really interested in. More specifically, the patient’s Originating sites must meet at least the following two requirements set out by Medicare:
Not all healthcare professionals are eligible to offer telemedicine services reimbursable under Medicare. Those who are eligible include registered nutrition professionals, registered dietitians, clinical social workers, clinical psychologists, clinical nurse specialists, nurse midwives, physician assistants, nurse practitioners, and physicians only.
Only HCPCS and CPT codes are covered for telemedicine reimbursements under Medicare. Check the full list of HCPCS and CPT codes eligible for reimbursement under telemedicine services. Remember these codes are updated on a yearly basis, which is why healthcare providers have to review them periodically.
As you might expect, not all types or forms of telemedicine services are eligible for reimbursement by Medicare. By definition, they only reimburse telemedicine services that mimic in-person care. In light of that, Medicare only covers live care services offered through telemedicine, and they meant to act as a genuine substitute for one-on-one doctor’s office visits.
In other words, covered services are those that involve real-time interaction between the patient and physician via video chat, video conferencing, etc. The interaction must meet security standards. Alaska and Hawaii are the only exceptions to this rule. In the two states, reimbursements are made for both real-time interactive services and store-and-forward telemedicine.
Like traditional healthcare services, Medicare will reimburse the provider for the eligible telemedicine services. But, on top of that, they will pay a facility fee to the Originating site. Medicare’s HCPCS Code Q3014 has everything you need to know about the facility fee for offering telemedicine services.
All states have some coverage for telemedicine under their Medicaid programs. However, there are no universal laws and regulations that govern telemedicine under Medicaid. That’s because Medicaid programs are operated by their respective states.
As such, reimbursement and coverage for telemedicine services under Medicaid vary greatly from state to state depending on the key policies in place in your state. If you want to keep abreast of what’s happening in the world of telemedicine and Medicaid programs, stay tuned to the American Telemedicine Association, the National Telehealth Policy Resource Center, and your state’s own Medicaid program site.
Nonetheless, here’s a rundown of what the CCHP says about telemedicine and Medicaid across America:
Even still, it is important to understand what to do to make sure that you get the most Medicaid reimbursement for health services offered via telemedicine. Here are some factors that you might want to keep top of mind because they affect telemedicine Medicaid coverage:
All these factors will determine how much reimbursement you’ll receive for telemedicine under your state’s Medicaid program.


By design, telemedicine was meant for remote and rural sites where healthcare facilities are understaffed and providers are unavailable or far between. The concept, however, can still deliver incredible benefits to those who live in urban areas where hospitals and healthcare professionals are accessible. After all, why would make a long trip to the physician’s office when you can get convenient care from the comfort of your own home?
This is not wishful thinking, though. More than 50 percent of American hospitals have already implemented RPM telemedicine solutions, which isn’t surprising considering that more than 12 million Americans are considered to be residents of remote sites.
Of course, that’s not all there’s to it. There are a myriad of advantages to telemedicine, and here are the top ones:
Access to quality health care is important to everyone. However, the location, travel time and distance between providers and the patient can have a huge impact on access. Luckily, one of the most pronounced advantages of telemedicine is that it gives patients increased access to medical information and healthcare specialists they may not readily be accessible to them.
Telemedicine can bring down both physical and specialist barriers to healthcare. For instance, patients in Rural Wyoming might not have access to oncologists in their local health centers. That’s where telemedicine can come to the rescue, offering them access to oncology specialists in other areas across the US.
During a live consultation with physician or specialists, be sure to ask important health questions and provide them with your medical history. So, this concept of digital health can especially benefit patients in healthcare underserved areas, particularly those in rural areas.
In a traditional health setup, care delivery usually ends after the patient walks out of the doctor’s office. With telemedicine, providers can keep a tab on their patient’s progress long after they leave their practices, do follow-up sessions for several days, and ensure that everything is okay.
Telemedicine puts a lot of technologies and avenues for follow-ups at the disposal of doctors – from live video conferencing tools to wearables that relay data on patient’s vitals and advanced remote patient monitoring systems.
Otherwise put, telemedicine and telehealth can help enhance the quality of patient care, as well as service delivery for all patients regardless of their location. And preliminary studies show that indeed telemedicine does improve the quality of care.
As a recent study, patients were more engaged in their health and care with telemedicine. Even more encouraging, the number of hospital admissions and readmissions dropped by 38 percent and 31 percent respectively.


Americans spend more on healthcare than any other nation in the developed world (or over $3.5 trillion annually to be precise). A significant chunk of this budget goes to unnecessary, administrative and avoidable spending, something that telemedicine has the potential of curbing.
More specifically, telemedicine can help spruce up the efficiency of healthcare delivery by curtailing issues like unnecessary doctor’s office visits and getting rid of administrative burden. It can also reduce non-adherence to medication, a menace that reportedly costs the US healthcare system up to $290 billion annually.
In addition to making physician’s visits more efficient, telemedicine can also reduce spending on travel and care for patients. Just by keeping non-emergency cases out of the hospital, it can save oodles of money for both the patient and provider.
In one recent study, medical analysts found that switching from inpatient care to telemedicine can save close to 20 percent for the American healthcare system.
In the past, patients left everything to do with their health to the doctors. Telemedicine is helping put the patient on the driver’s seat. This in line with the fact that patients now see themselves as consumers, and they want a high level of experience from their care.
Telemedicine is their best shot at the most quality experience. It allows them to connect on a more personal level with their physician, not to mention the increased frequency of telemedicine visits.
With more convenience and more opportunities to “see” the doctor, patients can leverage telemedicine to ask as many questions as possible, and get direct, one-on-one answers from trusted healthcare professionals. This ultimately boosts patient engagement and satisfaction, as well as empower them.
There’s no question today’s physicians are more burned out than ever before. By the same token, doctors are more stressed and less satisfied than ever. This can put a big bump on patient satisfaction and quality of care delivery, too.
Telemedicine could be the answer for the rising physician burnout. It can improve doctors’ job satisfaction by cutting down administrative work they have to do, and making meeting with patients effortless. Even better, healthcare professionals take advantage of telemedicine to strike a more robust work-life balance.


While the benefits of telemedicine are clear-cut, it is not without challenges and disadvantages. Some potential problems with telemedicine include a significant reduction in patient-doctor in-person interaction, issues with care continuity, lack of proper equipment, and technical training limitations. The elephant in the room, however, is the impending lawsuits that might arise from misdiagnosis, neglect, and whatnot.
Perhaps some of the biggest disadvantages are:
Patients may not have access to the services offered via telemedicine. Some doctor’s offices may also not have access to equipment and other solutions they need to offer telemedicine. Setting up and maintaining a telemedicine system from the group up is not small financial affair. Besides, telemedicine might also be too expensive for smaller, upcoming clinics and healthcare centers.
That’s not to mention the cost of training and educating healthcare providers so they can use telemedicine.
Yes, telemedicine makes it easier for doctors to provide patients with on-demand care. Any person can simply sign up for a telemedicine account, and use video conferencing to get their condition examined and diagnosis delivered right from where they are.
This approach can do wonders for patient experience. However, some telemedicine systems may cause issues and break down the continuity of care. Just imagine a situation whereby a new doctor is assigned to a patient he or she doesn’t have a full medical history. If there’s no link between the current physician and the telemedicine doctor, care delivery can take a hit.
(iii) Dealing with Reimbursement, Payment and Policy Changes can be Difficult
Navigating the reimbursement process in telemedicine space can be quite tricky. The provider has to worry about different laws and regulations that make it harder for them to understand the position of each state on telemedicine coverage.
While there are parity laws in several states that mandate private insurance companies to cover telemedicine services, Medicaid and Medicare are a different story. The doctors might be forced to get in touch with payers directly and inquire about their telemedicine reimbursement policies. This can be time-consuming and complex.
As if that isn’t complicated enough, most clinicians are paid a convenience fee between $35 and $125 per visit. That can be quite costly and confusing for patients under Medicaid, Medicare and those covered by private payers.
the other issue is that some people say that telemedicine robs patients of the much needed in-person interaction with their doctor, as well as full, one-on-one diagnosis. This, however, is something that is subject to debate. Of course, not all conditions and issues that patients warrant an in-person interaction.


Like all connected healthcare technologies, telemedicine is not immune to security and privacy risks. Cybersecurity issues like hacking can adversely impact on the patients’ and providers’ level of willingness and trust towards telemedicine.
Of course, these cybersecurity fears don’t come from a vacuum. The digital healthcare space has been plagued by several data breaches and privacy issues right from its inception. Here are a few stats that underscore the importance of building telemedicine systems with cybersecurity in mind:
88 percent of all ransomware breaches and attacks were primarily directed at the healthcare industry, with digital health taking the biggest hit.
According to a damning report by Ponemon Institute, $6.2 billion is lost by the US Healthcare system due to cybersecurity breaches. In response, it is estimated that the healthcare industry is planning to shell out over $65 billion to curb the menace and seal cybersecurity loopholes in the next half-decade.
Hacking account for 85 percent of all cybersecurity issues affecting medical records. That’s despite the fact that they make up only a quarter of all data breaches in the health space.
Against this background, it’s apparent that telemedicine carry a significant cybersecurity risk. Since medical records are some of the juiciest targets for hackers, telemedicine platforms have to be designed from the get-go for patient data to be protected.
Here are the principles that telemedicine developers and managers should consider when it comes to cybersecurity service:
The loopholes for cybersecurity breaches are too many to ignore when it comes to telemedicine. The patient can use a compromised or virus-infected machine, establish a connection via an insecure internet or accidentally share logins with the wrong people.
The risk of medical data being stolen, manipulated, hacked or changes in a telemedicine environment is simply astronomical. Here are some handy tips on how stakeholders can make sure to stay on top of telemedicine cybersecurity:
All communications between patients and doctors are subject to the Health Insurance Portability and Accountability Act (HIPAA). This also applies to the transfer, exchange, processing, and storage of patient information.
HIPAA has clear guidelines on how to make sure patient data integrity and security are ensured at all times. For a telemedicine system, there should be a designated HIPAA expert to see to it that cybersecurity measures are put into action to safeguard patient’s data. HIPAA officer or consultant can also do an A/B test for your telemedicine solution.
Even with a HIPAA officer onboard, you can use an extra set of eyes and hands to make sure your solution 100% tight as far as cybersecurity is concerned.
Once you have done an assessment of your telemedicine, it is crucial to zero in on any gaps that may threaten cybersecurity. Oftentimes that means checking for any loopholes in your cybersecurity measures. You will probably have to collaborate with your IT providers and bring in more measures to strengthen the security of your software, hardware, email clients, storage, cloud platforms, websites, and patient portals.
Leave no stone unturned. And involve every party, including doctors, IT vendors, etc. Don’t be afraid to get early feedback from potential patients.


Running a telemedicine practice is subject to a host of regulations, and HIPAA is probably the most important. What is it?
Short for the Health Insurance Portability and Accountability Act, HIPAA was signed into law in 1996 initially designed to reduce healthcare fraud and insurance fraud. That aside, HIPAA now guarantees the protection and secure handling of patient data, whether during submission, processing or storage.
There are two provisions of HIPAA that are most relevant and therefore applicable to telemedicine: the Security Rule and the Privacy Rule. And the reason is very obvious.
This is a short version of PEPHI, which sets forth the guidelines and framework for secure handling of patient information and data that are transferred or stored by electronic means. It encompasses 3 aspects of patient data protection that should be met by telemedicine to be compliant with HIPAA: technical, physical and administrative.
Privacy Rule clearly defines and sets the standards for the disclosure and use of PHO (Protected Health Information). All telemedicine providers that want to be in HIPAA compliance must develop and adhere to procedures/measures that will help in protecting and securing electronic Protected Health Information (ePHI). Whether traditional or telemedicine service, the Privacy Rule states that only the minimum medical info needed to care for the patient be shared or used.
To cut it short, the telemedicine system has to be HIPAA compliant, as well as all the staff, patients, and providers using the platform. As such, a telemedicine developer is not only required to develop a HIPAA compliant solution but also ensure that the company itself is run as per HIPAA regulations.
The part of HIPAA guidelines that is directed at telemedicine, therefore, directs that:
HIPAA compliance for telemedicine thus encompasses a strategic set of best practices that are documented, highly monitored and protected.


Are blockchain and telemedicine a perfect match? The pillar of blockchain lies in the technology’s ability to offer secure, immutable and decentralized transactions. In an increasingly trustless society, this might be fit for a new and exciting area of medicine and healthcare like telemedicine.
Blockchain in and of itself has a potential to reduce administrative, regulatory and operational issues associated with unifying our highly broken healthcare system to enhance delivery and patient care.
Given that 50 percent of healthcare organizations have adopted some form of telemedicine, it makes sense to bring in the blockchain. After all, a recent report shows that almost half of the organizations in the healthcare space are doing feasibility studies on whether or not to build blockchain into their business and operational models.
Why blockchain? There are plenty of benefits that blockchain brings to the telemedicine fold, which include:
It improves transparency. Today’s savvy patients crave transparency from their healthcare providers, especially when it comes to the quality of care, privacy and security of the medical information. They want to know who their medical data is shared with and why. The transparency that comes with blockchain technology bleeds into reimbursement and prescriptions.
Cybersecurity. When blockchain is used in tandem with certain cybersecurity measures, it can improve the security and integrity of electronic medical records systems. In other words, it helps remove the middleman from the equation.
Democratizing medical information. This is where telehealth and telemedicine converge in taking advantage of the decentralized nature of blockchain technology.
Helps with contracts and dealing with legal issues. Telemedicine is at the cusp of changing healthcare as we know it, but the new technology comes with some legal challenges. Due to the fact that blockchain records are immutable, this will reduce false patient claims and insurance fraud. It’ll also make it easy for telemedicine providers to stay ahead of government regulations.
There are several telemedicine solutions already onboarding blockchain technology. Take Myclinic.com, for instance. The telemedicine app which enables doctors to consult patients via video chat now accepts payment for services with cryptocurrency.


What if you could shop health care services just like everything else online? That’s exactly what Walgreens wants to offer to their mobile, online and in-store customers through Find Care Now. It’s a telemedicine platform-cum-marketplace which connects patients to a burgeoning selection of trusted healthcare professionals within Walgreens community.
Healthcareweekly covered the launch of Find Care Now comprehensively last year, denoting that Walgreens is a pioneer of telemedicine amongst large pharma retail companies. Indeed, the big-box retailer has always been at the forefront of innovation, and its foray into the telemedicine scene will expand the options that patients have when it comes to seeking health care via remote channels.
Part of the company’s Boots Alliance, Find Care Now brings a variety of healthcare providers closer to the patient, including traditional physicians, digital-enabled house call firms, telemedicine providers, and much more.
With Find Care Now, the patient can connect live with providers directly from the website or inside the app, establishing a one-on-one dialogue with the doctor. The best part is that the platform makes it easy for the consumer to know the exact cost of healthcare upfront.
Despite being a newcomer, Hello Alvin is one telemedicine company that already has everything going for it. The telemedicine provider allows patients with minor problems to connect with live physicians via video or phone in a matter of minutes.
Healthcare Weekly’s Codrin Arsene had a chance to sit down for a podcast with Joseph Truscelli, the CEO of Hello Alvin. From the conversation, it is clear that the visionary has the scoop on the ins and outs of the industry, as well as the future of telemedicine.
According to the CEO, The key differentiator for Hello Alvin is that they provide solutions to small businesses which doesn’t exist with most telemedicine providers.
The beauty of it all is that Hello Alvin is powered by one of the biggest names in telemedicine space: Teladoc. That means that their users have access to a huge range of healthcare professional under the umbrella of Teladoc.
Subscribers can opt for one-off remote visits, ongoing treatment or pick a monthly plan for as little as $20. For the standard virtual doctor’s consultations, you can expect to pay only $69 per visit.
MDLive is a telemedicine platform that has gained a lot of traction for treating skin problems, mild/acute conditions and mental health. It’s a 3-in-1 telemedicine system that allows patients to seek remote visits with physicians via a mobile app, as well as through a call center, or website.
The app is available for free download from the App Store and presents perhaps the most convenient and quickest way to establish a consultative dialogue with healthcare providers. You can use MDLive to seek virtual care for yourself or your loved ones.
The call center option is for phone-ins only. However, if you need live video consultation, you will be guided to download the mobile app or use the website. All up, the telemedicine platform makes it possible to “see” a doctor any time and any day of the week. In fact, you can expect a wait time of fewer than 15 minutes even during holidays.
The telemedicine system is even more robust and feature-rich from the provider’s end. Like with the traditional doctor’s office visit, a returning patient will be connected to a doctor they are most familiar with.
However, for on-demand consultations, there’s a smart algorithm that matches the patient with a physician based on the provider’s license, credentials, and patient’s location and needs. It all happens seamlessly in the background.
AmWell is one of the most popular companies as far as delivering top-notch telemedicine services is concerned. It’s a product of American Well, one of the most notable players in telemedicine, telehealth, and digital medicine.
It’s a direct-to-patient service supported by a mobile app, making it ideal for 24/7 availability with support for psychiatric, urgent care and an array of other non-urgent consults. They are all offered at a fixed cost so you know the cover up front.
According to American Well, AmWell is designed primarily to be a stop-gap health service. That means it is intended to provide diagnostic services in between normal physician’s visits, and shouldn’t be construed as an alternative to a doctor. Even still, the app gives the patient a chance to video consult with a licensed doctor.
As a patient, you can pick a physician of your choice based on availability. All conversations are recorded and presented securely and neatly on the patient’s profile for easy reference.
Babylon Health was one of the first telemedicine companies to add Artificial Intelligence and Big Data to their platforms. It operates AI Doctor, a telemedicine system that uses deep learning to match patients with the right healthcare service and provider based on their needs and other unique metrics.
As soon as the patient lands on the platform, they’ll meet AI bot which will ask a battery of questions to zero in on the issue at hand. Babylon Health off 24/7 support and availability to establish a conversation with the correct physician.
The platform allows consulting via video, text messaging and in-app communication with healthcare professionals. With a team of AI engineers, clinicians and scientists on board, Babylon’s Ai doctor is a slice of medical genius.
Lemonaid Health has established itself to become a reputable telemedicine company. It has built a responsible telemedicine platform that’s designed to offer virtual care services for sinus issues, weight management, birth control & reproductive health issues, and hair loss, just to mention.
The lemonaid app can help schedule a visit with an online physician on same-day and fixed-cost basis. With a partnership with a long list of pharmacists, they also provide a mail order delivery option for a number of medications.
Back in mid-2017, Lemonaid secured $11 million in their first Series A round of fundraising. Its team of healthcare providers includes clinicians, clinical advisors, patient care support team, physicians, and a CMO.
An on-demand telemedicine service, Doctor on Demand defines itself as a healthcare practice that established a live connection with board-certified doctors and patients. The patient can garner face-to-face access to a trusted provider in a matter of minutes via a mobile app or website.
The telemedicine startup secured a $74 million funding, placing it under the public radar. Even then, their app had gained more than 1m downloads on Google Play. It’s now a nationwide provider of telemedicine services in each and every 50 states.
The primary goal of Doctor on Demand is to connect every patient to quality care via telemedicine, regardless of their location or health insurance status. What makes this platform stand out is their video call quality, which boasts over 98 percent success rate.
The telemedicine system providers nationwide access to a diverse selection of providers, including family practitioners, internists, EM professionals, pediatrics and general practice doctors. They also have a booming mental health practice.
First Opinion offer telemedicine service via an app that is only available from the App Store. It has become well-known for the fast response times, and selection of online doctors. With a robust messaging service, you can get sound medical advice, get diagnose and fill prescriptions in no time.
LiveHealth is a telemedicine app that makes interactions with your physicians much more convenient and effective. LiveHealth features all of the patient’s medical records under one place so they can track their health and get necessary care in due time.
Teladoc is a veteran in the world of telemedicine, having been around for over 15 years. It started by offering their virtual medical services to self-insured employers but now cater to those covered under Medicaid, Medicare and private health plans.
In 2017 alone, Teladoc did over 1.4 million visits. They offer a 24/7 customer service, as well as an app available for Android and iOS devices, fully-fledged website, and portal for managing patient data.
Just recently, Teladoc health built a first of its kind pediatric telemedicine platform in collaboration with Cincinnati’s Children’s Hospital. Other telemedicine providers like Hello Alvin are powered by Teladoc.
The company is known for performing routine quality assurance tests with a reputable team of healthcare professionals. The team reviews patient charts to make sure they are receiving top-of-the-range quality, care, and experience.


Like everything that touches on the health of Americans, telemedicine systems are supposed to comply with a battery of laws and regulations at both state and federal levels.
The proliferation of telemedicine and its increased adoption by small & large health systems, hospitals, and private practices has forced lawmakers to come with a ton of legislation related to this emerging concept of medicine.
Get this: more than hundred telemedicine-related bills were tabled in the first month of 2015 alone. Today, all states and relevant health authorities have policies in place to govern telehealth and telemedicine.
Medical associations like HSTA, AMA, and FSMB have also continued to craft the basic regulatory framework and guidelines for telemedicine practice. HIPAA is also at the forefront of telemedicine regulation.
However you look at it, telemedicine providers, developers, and healthcare organizations have to stay on top of these pieces of regulation lest they find themselves on the wrong side of the law.
Because of programs like Medicare and Medicaid, most states have had to implement laws, regulations, and guidelines for telemedicine practices. More specifically, their medical boards have laid out the necessary standards for healthcare providers within respective state jurisdictions.
The key mission of FSMB (Federation of State Medical Boards) is to ensure that providers that offer care via telemedicine uphold similar standards as they’d when offering in-person care at a doctor’s office. It is anticipated that all states will join in soon. Here’s FSMB’s comprehensive doc on state-by-state telemedicine practice administrative and regulatory requirements.
As we’ve stated earlier, not all states recognize or reimburse all three types of telemedicine. The Medicaid program for Alaska, for instance, reimburses for store-and-forward telemedicine, while Arizona telemedicine regulations don’t provide for this requirement.
Parity laws have the most impact on telemedicine coverage. It mandates that private insurance companies (payers) should cover telemedicine practice, though particular restrictions and policies on reimbursement are usually different from state to state.
At the moment, the District of Columbia and 31 US states have ratified parity laws for telemedicine reimbursement. Although most states laws aren’t often clear, most private payers reimburse at the same level as coverage for in-person care. In some instances, parity laws might also influence telemedicine practice coverage under the Medicaid program.
According to most state regulations and current federal policy, telemedicine practices may be required to obtain informed consent from the patient. While some states may have no requirements at all, some will need a patient’s written or verbal consent. All in all, it’s crucial for telemedicine practices to educate their patients about their services, quality, reimbursement and what they should expect.
In recent years, almost all states have legislated regulations on online prescribing of medication. These regulations usually focus on medication for managing chronic pain and scheduled drugs, especially opioids.
A handful of states make it mandatory for the patient to appear in person for a physical test to obtain online prescriptions via telemedicine legally. Therefore, it is paramount for telemedicine practices and patients to get conversant with individual state’s laws and regulations on online prescribing before they embark on telemedicine.
By virtue of definition, telemedicine platforms should make it easy for patients to receive services and care from cross-state providers. This is made possible by cross-state licensing regulations.
Not all states have licensing agreements with other states. So, telemedicine providers to check if their states do have mutual recognition, which is a system whereby the licensing bodies in each state (usually the state medical board) enter into an agreement to accept the legal processes and policies of the originating state.
While not all states have this regulation, some of them mandate that any telemedicine visit should involve a patient-physician pair with a pre-existing relationship. Oftentimes that means that the patient and provider are required to have had one or more in-person consultation prior to telemedicine visit.


Telemedicine is no longer a futuristic concept, but an area that has the potential to revolutionize care access and delivery. It meets patients via multiple convenient channels and delivers care to where they are.
Over the years, better technology has helped make telemedicine easier to use, more affordable and more accessible for providers and patients alike. With the advent of more agile, more cutting-edge and snappier technologies like AI, IoT and Big Data, the future of telemedicine is brighter than ever.
We are also likely to see unified adoption of telemedicine in conjunction with telehealth. Quick peek at the stats on the future growth of the industry show that telemedicine will cause a massive shift in how consumers view and get care.
With the widespread push for regulation changes, here are some key talking points you need to know about the future of telemedicine:
In 2015, Medicare spends about 0.01 percent (close to $15 million) of its total healthcare spending on telemedicine services. That’s poised to change in the near future as adoption continues to be seen across the spectrum.
More states will introduce telemedicine-friendly regulations, especially when it comes to their Medicaid programs, and it’s not hard to see that. Medicare coverage of telemedicine services will also most likely see expansion sooner than later.
In November last year, technical and policy changes to Medicare Advantage were introduced. In specific, Section 50323 and Part B will append additional benefits for those seeking telemedicine services by 2020.
Fresh statistics show that chronic disease management is a key potential area for telemedicine adoption. This is an untapped market that is expected to fuel acceptance and coverage of telemedicine, according to Cleveland Clinic.
Because patients living with chronic diseases often make frequent trips to the doctor’s office, telemedicine companies will most probably target this patient population. It’s a win-win. Increased use of telemedicine will result in a decreased number of ER and physician’s office visits, as well as lower hospital admission and readmission rates.
Hospital-at-home is a model of telemedicine where patients who could be hospitalized can instead be treated at home. This usually applies to patients suffering from chronic diseases like heart failure, pneumonia, COPD, and so forth.
A growing number of studies has revealed that hospital-at-home telemedicine services can help cut costs, reduce delirium rates, and shorten treatment periods. It can also lead to a reduction in hospital readmission rates.
There’s no turning back for telemedicine. And experts predict that telemedicine visits will increase by a significant margin in the next couple of years. According to a Tractica report, telemedicine video consults will reach close to 160 million annually by 2020.
Another conservative report by Mordor Intelligence states that telemedicine market will be worth a whopping $66 billion by 2021. As digital health take shape and goes mainstream, we can expect the demand for telemedicine services to grow at a breakneck pace.
The increased demand for digital health platforms will allow the market to continuously grow at a rapid pace. Of course, there are a few barriers that might hold back complete its complete adoption.
Today’s healthcare space is faced with enormous care delivery challenges. There’s an increasingly urgent need for lasting solutions and strategies to help lower healthcare costs, improve quality of care, and expand care access. Telemedicine is a field of modern medicine that checks all three boxes.
Together with telehealth, telemedicine can help pave the way for a health wide improvement, which is why it is expected to cause major shifts and revolutionize healthcare.
In spite of this, telemedicine and telehealth should not be confused. Telehealth refers to means, methods, and strategies for improving healthcare support, medical education and public health. It entails a collection of electronics, telecommunication technologies, and services that are used to support and provide long-distance support.
Telemedicine refers to the use of telecommunication technologies and medical information to support and deliver care to long-distance patients.
Despite the recent wave of popularity, telemedicine isn’t actually a new idea. The use of the telephone to deliver care to remote or otherwise inaccessible areas has been broached since the 18th century.
It wasn’t until the 1950s that it was primarily used by university medical centers and large hospitals to reach patients in remote locations. Today, over 90 percent of American consumers have a positive view of telemedicine.
With that being said, the telemedicine market is currently at the cusp of unprecedented growth. In fact, recent stats show that the market will be worth around $130 billion by 2025, at a CAGR of 19.2 percent from $18 billion in 2015.
That in and of itself should not come as a big surprise because telemedicine offers a system-wide benefit. These advantages include:
Increased access to care for patients, especially those located in remote and rural sites where healthcare facilities are scarce and understaffed.
Telemedicine makes it easy for patients to access specialist providers. These include oncologists and other healthcare professionals that are in high demand.
It can help reduce healthcare costs for both providers and the patient. By reducing no-shows, replacing walk-ins and decreasing administrative costs, telemedicine can truly change healthcare as we know it.
It can also improve care quality. Doctors can now focus on diagnosing and treating patients rather than worrying about the administrative side of care. On the same note, this can help reduce physician burnout and spruce up their job satisfaction.
How does telemedicine work? It helps establish a variety of connections that will improve care access, quality of service and delivery. This can be achieved through e-health patient service websites, monitoring center links, point-to-point connections, and networked programs.
In saying so, there are four main types of telemedicine, and each can affect reimbursement and care delivery. These are mobile health platforms, real-time interactive services, remote patient monitoring, and store-and-forward telemedicine.
Thanks to increased adoption, there are numerous conditions currently covered by telemedicine. These include telepsychiatry, dermatology, cold or cough, oncology (cancer treatments), blood pressure problems, post-surgery follow-ups, online prescribing, digestive problems, rashes, addiction, sore throat, and much more.
What about reimbursements? Telemedicine is recognized and reimbursed by Medicare, but the level of reimbursement varies by state. Medicare will only reimburse telemedicine services in which the Originating site is within a Health Professional Shortage Area (HPSA), and the provider must be eligible too.
Medicare coverage of telemedicine is also affected by medication prescribed, applicable codes, eligibility of the healthcare professional, and whether facility fee is going to be paid.
Talking of Medicaid, programs in 48 states now cover live interactive telemedicine services, while 12 cover store-and-forward telemedicine. 19 state Medicaid programs reimburse telemedicine services offer via remote patient monitoring. Currently, only 8 states cover all 3 types of telemedicine.
Telemedicine is not without challenges and downsides. The biggest risk is cybersecurity issues, followed by cost and availability, as well as reimbursement problems.
Even still, the future of telemedicine is brighter than ever. It is expected that the market will grow at a fast pace on the back of continued adoption, increased technology, and enactment of more favorable regulations.