



Get new exclusive access to healthcare business reports & breaking news




Rheumatoid Arthritis (RA) is a systemic autoimmune disease that affects less than 1% of the U.S population. It’s also more common in women, with nearly three times more women diagnosed with the disease than men.
Though this condition can carry serious complications if not diagnosed early, its symptoms often make it difficult to identify. Many people may mistake it for other forms of arthritis. It may also be misdiagnosed because its symptoms vary.
While more awareness has been raised in recent years, many are still unaware of what rheumatoid arthritis actually is, and how it differs from ordinary types of arthritis.
This article will help you learn more about rheumatoid arthritis and provide you with the information you need about the condition.
Starting with the basics, you’ll learn what the condition is before understanding its symptoms, causes, risk factors, and treatment options.
By the end of this article, you’ll have a comprehensive understanding of the condition that enables you to work with your medical professionals, or help someone you know if they feel they may be suffering from the condition.


This attack causes inflammation in and around joints, and makes tissue lining the joints (the synovium) thicken. This is visible through swelling of joints, and sufferers often experience pain in and around these areas.
Although rheumatoid arthritis can affect any joint in the human body, it most commonly affects hands, feet, wrists, elbows, knees, and ankles. It also usually occurs bilaterally, meaning if one hand or foot is affected, the other one probably is too.


In the early stages, someone with this condition is likely to experience minor symptoms that come and go, which is why misdiagnosis is common.
The main difference between rheumatoid arthritis and other conditions its commonly mistaken for is that these symptoms affect both sides of the body. They will also progress over a period of weeks or months.
In addition to this, it’s important to remember that, as with many chronic conditions, it’s usual for symptoms to increase and decrease in frequency over time.
Someone experiencing significant bouts of symptoms is likely to be experiencing a flare up, where the condition is considered ‘active’ and has a bigger impact on day-to-day life.
This isn’t permanent, however, and a sufferer of the condition is also likely to experience periods of inactivity or remission, where symptoms may be less noticeable.
As mentioned, symptoms of RA vary from person to person, but below are some of the most common ones that affect sufferers.


Though this is most commonly associated with periods of sleep, it can also occur as a result of inactivity from prolonged sitting or napping.
Those who experience this symptom will generally find they have difficulty with moving the joints on either side of their body for some time after waking up.
Although this symptom in itself can point to several types of arthritis, rheumatologists consider it a key sign of rheumatoid arthritis in particular when it lasts at least an hour.


Usually, this symptom starts in the joints of the hands and comes on slowly. In some cases, however, sufferers can be completely fine one day and find several joints are stiff the next.
Unlike morning stiffness, general joint stiffness can occur at any point in the day and isn’t affected by how active or inactive you are.


This is described by patients as an aching or throbbing pain that is usually worse after inactivity but can occur constantly or randomly at any point throughout the day.
This symptom is also likely to be bilateral, and though it usually begins in the fingers and wrists, people may also experience it in their knees, ankles, or shoulders.


Although you may notice a difference in size from the start, swelling is usually minor when this condition first develops and is usually associated with the warmth of the joints.
As the condition progresses, or as the result of complications, some people may also develop small but hard swellings called rheumatoid nodules that grow under the skin around affected joints.


Fatigue won’t affect everyone with rheumatoid arthritis, but studies have shown it is prevalent in up to 80% of cases.
For those who experience it, fatigue is often accompanied by a general feeling of ill health, and the levels at which it affects someone can vary on a weekly or even daily basis.
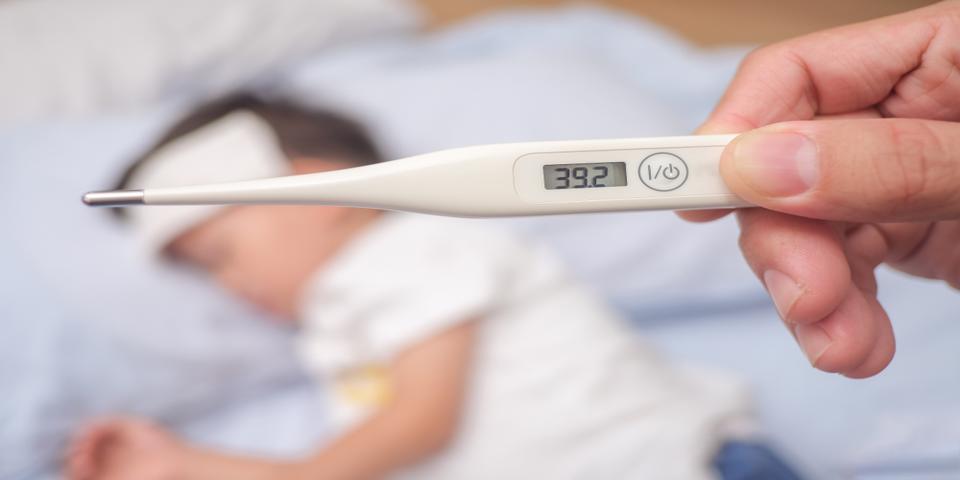
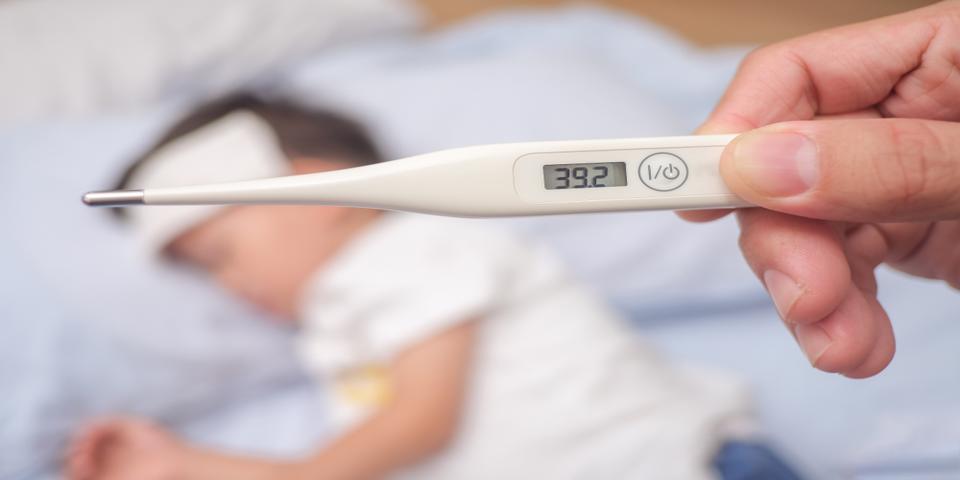
But low-grade fevers in addition to other symptoms can be a key warning sign of the condition.
They occur because rheumatoid arthritis can also affect the body’s organs, leading to widespread inflammation and fevers.


This is why some people, especially if their condition has worsened before seeking treatment, may experience numbness or tingling in some areas of the body.
This inflammation can also lead to other symptoms, like a burning feeling in your hands if a condition like carpal tunnel syndrome develops.
You may also experience a squeaking or crackling sound coming from the joints of your hands and feet as a result of damaged cartilage grinding against joints when you move.


Over time, the inflammation causes tendons and ligaments to become unstable and weak, making it harder to move certain joints freely.
It may even develop to a point where you are unable to bend or straighten some joints at all.
Your range of motion can also be negatively impacted by pain, a common symptom of rheumatoid arthritis.
Despite this, it’s important to engage in regular, gentle exercise to try to maintain your range of motion as much as possible.


So far, researchers have determined that the disease is an autoimmune condition that occurs as a result of an imperfect immune system.
This condition causes the immune system to incorrectly attack the joints, and leads to inflammation that can spread around the body.
While no definitive cause has been determined, researchers are looking into links with genetics, hormones, and environmental factors.
There are also potential risk factors that may increase your risk of developing the condition, which we will discuss later in this article.


This is primarily because the inflammation of RA can cause significant problems when it goes unchecked, with the potential for serious complications.
The severity of these complications can be decreased if you seek treatment as soon as you notice symptoms occurring.


If this occurs, irreversible damage to the joints may occur, making it harder to maintain your range of motion and remain pain-free during periods of remission.
In addition, you may also develop firm swellings called rheumatoid nodules, which can create visual deformities on various joints within your body.
The best way to avoid this is to seek treatment as soon as you notice symptoms of rheumatoid arthritis, especially if these symptoms involve swelling or pain in certain joints.


This is because the joint swelling leads to damage to tendons, ligaments, and muscles, all of which help keep joints stable.
When these are damaged, the joints become weaker, leading to a permanent loss of function that is ordinarily irreversible.
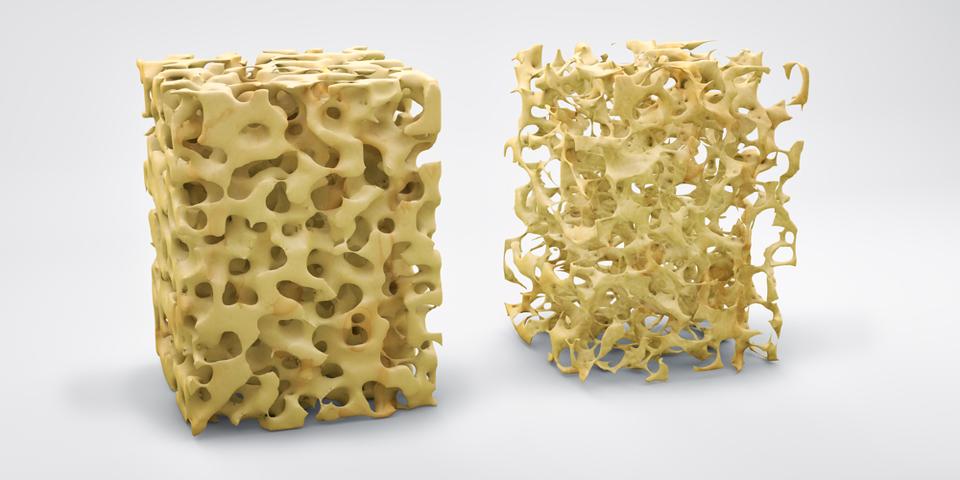
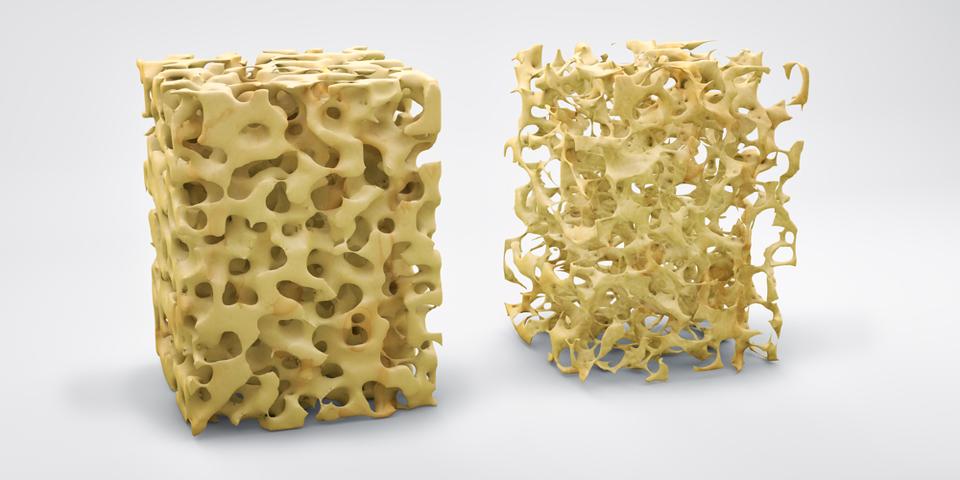
Although it ordinarily affects older people, even younger people can develop bone loss from chronic inflammation caused by untreated rheumatoid arthritis.
Joint damage, another complication mentioned above, may also lead to reduced physical activity, which also increases the risk of developing osteoporosis.


The Arthritis Foundation says that rheumatoid arthritis patients are at an increased risk of developing coronary artery disease because of systemic inflammation.
The inflammation that attacks the synovium–the tissue surrounding the joints–can also spread to other organs, such as the heart.
In particular, it’s thought that this affects the endothelium, the innermost layer of blood vessels. When the endothelium is inflamed, the lining of the blood vessel is damaged and allows plaque to build up, leading to coronary artery disease.
In cases of untreated rheumatoid arthritis, this risk of coronary artery disease increases because the inflammation is not controlled and affects the blood vessels.


Anemia, a condition that occurs when the body lacks enough red blood cells, commonly occurs with rheumatoid arthritis patients.
If rheumatoid arthritis is untreated, its chronic inflammation decreases the formation of blood cells in the bone marrow further.
With a diagnosis, doctors are often able to treat inflammation early, preventing anemia or lessening the severity if it does become a problem.


This is largely due to the various complications involved with chronic inflammation, with around 25% of sufferers dying from cardiovascular disease. Another substantial amount also die from infections that can be directly traced back to this condition.


In fact, the inflammatory process of the condition on the brain and nervous system can produce neuropsychiatric symptoms, like depression.
Depression is also common in patients with untreated rheumatoid arthritis because of the loss of independence and the disabling aspects of chronic inflammation.


While the understanding of what causes rheumatoid arthritis is extremely limited, researchers have been able to identify several genetic and environmental risk factors.
These have resulted in groups of people with the same characteristics, as listed below, identified as being at higher risk of developing the condition.


Rheumatoid arthritis isn’t a condition of one age group; anyone can develop it at any time.
However, your risk does increase with age, with older adults in their sixties considered to be most at risk.
Interestingly, people under 40 are considered to be least at risk of developing rheumatoid arthritis, with cases far rarer than in older people.
If it occurs at a younger age, it’s considered an early onset of the disease and is diagnosed as juvenile rheumatoid arthritis.


According to current diagnostic information, women are more at risk of developing rheumatoid arthritis than men.
In fact, the current diagnostic ratio stands at three women for every man and has remained relatively unchanged since being identified.
There have been a few hypotheses of why more women than men are diagnosed, but the most likely is that women are more susceptible to autoimmune diseases in general.
Although we do not currently fully understand why some researchers believe it may be related to hormones or the menstrual cycle.
Although women are already at an increased risk of developing rheumatoid arthritis when compared to males, this isn’t where it stops.
The Centers for Disease Control and Prevention (CDC) reports that women who have never given birth may be at greater risk of developing the condition.
Unfortunately, there is currently little research to explain this, though it could be linked to hormonal factors.


Genetics has been a key area of interest in research on the causes of rheumatoid arthritis, and studies are beginning to show links.
In fact, advances in technology and the increased use of genetic studies have helped identify more than 100 genetic markers that may be linked to rheumatoid arthritis.
Twin studies have also revealed a potential hereditary component to rheumatoid arthritis in at least 60% of cases.
Despite being a risk factor, however, genetics cannot be cited as a cause, as genetics don’t account for 100% of cases identified.
Some researchers believe that your genetic background is only a risk factor, and that environmental factors trigger certain genetic markers and cause this condition to develop.


Smoking has been identified as an environmental risk factor that could trigger those who are genetically predisposed to developing rheumatoid arthritis.
It’s thought that smoking over long periods, twenty years or longer, triggers faulty immune functioning which may cause the abnormal immune response seen in rheumatoid arthritis.
Those who already have this condition also increase their risk of worsening symptoms and reducing time spent in remission, as smoking can make treatment options less effective.
It can also discourage people from engaging in activities that directly improve their condition, like exercise.


One of the pioneering studies that looked into this found that adverse childhood traumatic experiences could greatly increase the future risk of developing rheumatoid arthritis.
There were 10 different types of trauma tracked, including abuse, neglect, domestic violence, mental illness, or substance abuse in a parent, and divorce.
If someone had just two of these factors in their childhood, it was found that they were more than twice as likely to be hospitalized for rheumatoid arthritis or other autoimmune disease.
It’s also thought that children with lower-income parents are at an increased risk of developing rheumatoid arthritis as adults, though we don’t currently understand why.


We are constantly being told about the health-related dangers of carrying additional weight, but very few people know that it also increases their risk of developing rheumatoid arthritis.
Even if you are only a little overweight for your height, you could be at a higher risk of developing the condition than if you are in the healthy weight range.
This risk increases the more overweight a person is, meaning someone who is obese or morbidly obese is significantly more likely to be diagnosed with rheumatoid arthritis.


Although some primary physicians will perform the basic examinations for rheumatoid arthritis, many will refer you to a specialized rheumatologist if you have symptoms.
This is because it’s very difficult to be diagnosed in the early stages, and it takes a specialist to separate your symptoms from other autoimmune diseases and forms of arthritis.
At this initial appointment with a rheumatologist, they will likely ask about your medical history and recent symptoms.
This can help them determine whether you have risk factors for rheumatoid arthritis, and also whether your current symptoms are consistent with those of rheumatoid arthritis.
After this, they will likely perform a physical exam, where they check each joint looking for tenderness and swelling, as well as painful and limited movement. They will also look for patterns in joint pain because rheumatoid arthritis affects both sides of the body equally.
Depending on the severity of your symptoms, they may also look to see if you have begun developing the signs of a late diagnosis, such as rheumatoid nodules or a low-grade fever.
If these examinations have been carried out, you will be referred to have one or both of the tests discussed below to confirm your condition.


Blood tests are the first port of call for most rheumatologists, as they can be used to measure inflammation levels. In patients with rheumatoid arthritis, this presents itself as elevated ESR rates or C-reactive proteins.
This blood test may also be used to look for anti-CCP antibodies, the specific type of antibodies associated with rheumatoid arthritis.


If you are showing signs of advanced rheumatoid arthritis, your rheumatologist may also recommend an X-ray, ultrasound, or MRI to look for joint damage.
This can include erosions, which is the loss of bone within specific joints and narrowing of joint space altogether.
Even if you are in the early stages and these warning signs aren’t present, these tests can be used to determine the progress of your condition over time.


There is currently no cure for those suffering from rheumatoid arthritis, but there are several treatment options that can help people experience longer periods of remission.


Medication your doctors prescribe depends on the severity of your symptoms and how long you’ve had the condition. There are four different types that you may be given, which include:
These are nonsteroidal anti-inflammatory drugs that are used for reducing inflammation and relieving pain.
You can buy this without a prescription in the form of ibuprofen and naproxen sodium, but your doctor may also prescribe stronger ones if you need them.
Corticosteroids such as prednisone are man-made versions of hormones normally produced in the adrenal glands and act to reduce inflammation.
They are used when NSAIDs fail to provide relief for reducing inflammation caused by rheumatoid arthritis, which reduced pain and slows joint damage.
These medications are usually provided temporarily to deal with acute symptoms during flare-ups, and patients gradually taper off steroids once symptoms subside.
Although there is no current cure for rheumatoid arthritis, DMARDs like methotrexate, leflunomide, hydroxychloroquine, and sulfasalazine can slow the progression of the disease.
The use of this medication increases your chance of saving joints from being destroyed or disfigured by rheumatoid arthritis and may save the tissue surrounding them.
Biologic agents, otherwise known as biologic response modifiers, are a newer subtype of DMARDs that specifically target parts of the immune system that trigger inflammation.
They help to prevent joint and tissue damage, but are rarely prescribed because when taken in large doses, they may have serious side effects like blood clots in the lungs.
When they are prescribed, you will usually also be prescribed a non-biological DMARD alongside, like methotrexate.


In addition to suggesting medication, your rheumatologist or primary doctor may also refer you to a physical or occupational therapist.
A physical therapist can help you with exercises that will keep your joints flexible for as long as possible.
Your occupational therapist may also help with this, but their main role is to help you find new ways to do daily tasks so you are putting less strain on your joints.
This might include providing you with different assistive devices that help you maintain independence, such as handgrips for sharp knives and cutlery.
They may also recommend that you avoid wearing certain clothing, like shirts with buttons, or provide you with devices that can help in that area, too.


Surgery is usually an option that is only suggested when medications have failed to prevent or slow joint damage and you have severely damaged joints.
If your condition is considered severe and your joints are already disfigured or painful at the time of diagnosis, surgery may be considered early on in your treatment plan.
There are four types of surgery that you can have for rheumatoid arthritis. These include:
This surgery involves removing the inflamed synovium lining that surrounds your joint to relieve pain and increase your range of motion.
This surgery may be recommended if you are experiencing problems with your knees, elbows, wrists, fingers or hips.
As previously mentioned, complications of rheumatoid arthritis mean the tendons around your joint may loosen or rupture.
This is not only painful but it can be dangerous because it makes the joint itself less stable.
Depending on the damage, a surgeon may be able to repair the tendons, which is when you would be recommended for this surgery.
If your joint has come out of alignment, is considered unstable, and you aren’t a candidate for tendon repair surgery, fusing your joint may be the next best option.
It’s also offered as a pain-relieving option for situations where a full joint replacement may not be recommended.
A more complicated surgery available for rheumatoid arthritis, total joint replacement involves removing a damaged major joint.
A replacement joint made of plastic or metal is inserted and the new joint then functions like your old one.
These are most commonly done on hip and knee joints, but your specialist may also recommend this surgery for another joint if it seems appropriate.


Although lifestyle changes aren’t going to be enough on their own, they can help to optimize the results from other treatment options, such as medication.
The primary change is exercise, and engaging in regular, gentle exercise helps strengthen the muscles around your joints and may also help fight fatigue.
Consider consulting your doctor before doing this, however, as exercising on tender, injured or inflamed joints may do more damage than good.
You can also help yourself by finding ways to relax, as some people find reducing stress can also help them manage their pain.


Although there are many alternative treatment adjuncts, there are three that many in the rheumatoid arthritis community use. These include:
Many people with rheumatoid arthritis include fish oil as part of their daily supplement routine.
Some studies have shown that it may reduce pain and stiffness, but these studies are still in their preliminary stages.
Fish oil can interfere with some medications, so if you are considering this, it’s worth checking with your doctor before you do.
Like fish oil, the seeds of plant oils such as evening primrose, borage, and black current can help with rheumatoid arthritis morning stiffness.
In addition, some studies have shown that plant or essential oils may reduce pain.
Because these oils can also interfere with other medications and, in rare cases, cause liver damage, it’s a good idea to check with your doctor before beginning use of these oils.
If you aren’t one for supplements, engaging in Tai Chi is another form of alternative medicine you can try.
The practice combines gentle exercises and stretches with deep breathing, which has been proven to relieve stress.
Not only can this help you to control pain, but it may also help to improve mood, helping to combat the common rheumatoid arthritis side effect of depression.
Rheumatoid arthritis is an autoimmune disease that occurs when the immune system mistakenly attacks the joints.
This causes inflammation in and around joints, leading to swelling and pain, and tends to affect both sides of the body equally.
With a chronic condition like this, symptoms come and go through a system of flare ups and inactivity, and affect everyone differently.
These symptoms vary from stiff and painful joints to fatigue to neuropsychiatric problems like depression.
It’s important to remember that rheumatoid arthritis symptoms do mimic those of other conditions, but knowing the risk factors can help you determine whether rheumatoid arthritis is possible. These include factors like age, sex, and genetics.
If you think you have the condition, however, it’s important to seek a diagnosis; not doing so can lead to complications that make your life extremely difficult. In addition to this, it can increase your risk of mortality.
Some consequences, like reduced function and deformities in joints, might be fixed with surgery, but others like osteoporosis and coronary heart disease could affect you for the rest of your life.
When you experience these complications, or in cases where your diagnosed rheumatoid arthritis has worsened, other treatment options like therapy or medication may be suggested.
These are put in place to help improve things and give you the best quality of life possible, despite the difficulties that rheumatoid arthritis can pose.
At the end of the day, the best way to have a positive outcome when you have rheumatoid arthritis is to seek a diagnosis as early as possible. This process is relatively fast, beginning with your doctor and ending with blood and imaging tests from a rheumatologist to confirm your condition.